We’re all familiar with the flu. Most consider it a pesky inconvenience or perhaps a good reason to miss work to stay home and watch Netflix. Among the list of viruses frequently mentioned in the news — Ebola, HIV, Zika — the “scare factor” associated with the flu is relatively low. But to an epidemiologist, the influenza virus is both frightening and a very real, impending threat. Indeed, scientists have been saying for the past decade that the “next big one,” (i.e. the next highly pathogenic, pandemic flu strain) could emerge at any time, and when it does, it’s going to be bad.
Determining the Most Deadly Flu Strains
The virulence of flu strains waxes and wanes over time. Influenza viruses accumulate mutations that alter their infectivity, and new strains emerge periodically, often in seasonal patterns or waves. The flu that infects many people each winter tends to be a virus that is just different enough from the previous year’s predominant strain to establish infection and typically causes minor symptoms. Occasionally, however, a new strain will emerge, either from recombination between two human strains, or from an event called “spillover,” in which an animal virus mutates in such a way that it becomes able to infect humans. These are the strains that epidemiologists are most worried about, for several reasons.
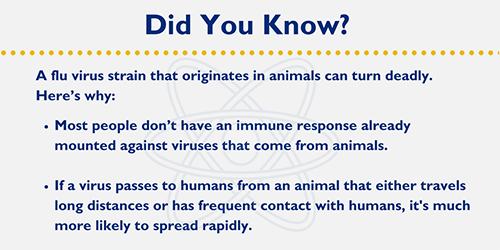
First, a recently crossed-over virus tends to be more virulent to humans because it is sufficiently different from previously-encountered strains that most hosts don’t have an adaptive immune response already mounted against it. Second, if a recently crossed-over virus is spread by an animal that travels long distances (e.g. birds), or has frequent contact with humans (e.g. pigs), this increases the potential for the virus to spread rapidly, not just via human-to-human transmission but also animal-to-human. Indeed, scientists believe that the most virulent influenza strain in recorded history — the Spanish flu — resulted from a crossover event from an avian virus, with the result being a pandemic that killed more people than were killed throughout the entirety of World War I.
It’s safe to say that most people alive today don’t remember the last “big one.” The worst pandemic in recorded history took place between September 1918 and April 1919, during which the virus killed an estimated 675,000 people in the United States and as many as 50 million people worldwide. In more recent flu outbreaks, most deaths are people from at-risk populations — children, the elderly, and people with compromised immune systems — whereas healthy adults are typically considered to be less at risk. For reasons that are still not well understood, the virus that caused the Spanish influenza pandemic specifically killed young, healthy adults at a much higher rate than has been seen before, or since, such that 50 percent of deaths were people between the ages of 20 and 40, and 99 percent were under the age of 65.
The virus ultimately infected 25 percent of the U.S. population and as much as 40 percent of people worldwide, making it the most infectious flu strain in recorded history. Although in the U.S. only 2.5 percent of infected people died, which admittedly doesn’t sound like much, this value is several-fold higher than the case fatality rates of other flu strains. This seemingly low fatality rate (for comparison, the recent epidemic strain of Ebola had a case fatality rate of approximately 50 percent) lowered the average life expectancy in the U.S. by 12 years.
The Only Certainty is the Uncertain
With past pandemics in mind, epidemiological experts pay close attention to each year’s flu strains and broad trends across time to try to predict when the next big one will hit. Increasing population densities, advances in air travel and the globalization of business in the last century make it extremely likely that when it does hit, it will impact the world more greatly than the Spanish influenza pandemic. Indeed, it has been estimated that if a strain infected and killed the same percentage of people as in 1918, today, somewhere between 74 and 370 million people would die.
Unfortunately, the inherent unpredictability of viral mutation and crossover events means that it is unlikely that researchers will be able to head off such an event with prospective vaccine development, and predictive modeling based on past flu pandemics has failed to identify any concrete patterns. In the meantime, epidemiologists are stuck waiting, with the unsatisfying reality that, as the philosopher Pliny the Elder said, “the only certainty is that nothing is certain.”
Related Content
- The Zika Virus: What You Need to Know
- The Flu: 3 Ways to Fight Back at 50-Plus
- A Parent’s Guide to the Flu