The term “doctor” can be traced to its Latin root, docēre, which means “to teach.” And indeed, teaching is ubiquitous in medicine; the residency system that trains physicians is grounded in intensive teaching and learning. Moreover, educating patients about their conditions is a primary objective for every doctor.
But five years ago, I was involved in a different style of education: teaching high school. During that time, I learned invaluable lessons that have also been pertinent to my time in medicine. Below are three takeaways from teaching high school that I continue to keep in mind every day at the hospital.
Lesson 1: Everyone has a story.
During the second week of my first year teaching, one of my students threw his classmate’s backpack across the room and shattered several graduated cylinders. Before I could react, he stormed out of the classroom. When I eventually caught up to him in the hallway, I learned that he had only been eating the one meal provided by school each day due to financial difficulties at home and was unable to concentrate in class because he was so hungry. It was only after his classmate waved a bag of snacks in front of him mockingly that he lost his temper. In this situation, if I had simply addressed the student’s behavior based off the isolated incident in the classroom instead of taking the time to listen to his story, I would have been unable to address his core issue and actually help him.
Likewise, in the hospital, the quick snapshot of what we learn in a single patient interview rarely tells the entire story. Oftentimes, medical care requires us to go beyond single visits and identify what happens outside of the hospital or clinic to adequately address a patient’s health concerns. It is important to remember that every person has their own circumstances and experiences that inform their current presentation, despite how simple their medical case may seem at first glance.
Lesson 2: Your mindset is important.
When first starting out as a teacher, I saw a flow diagram similar to the one below:
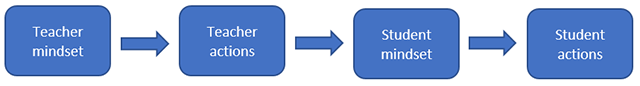
The concept is simple but incredibly powerful; Your mindset should always inform your actions. Unfortunately, in many professions — including teaching and medicine — it is frighteningly easy for experience to eventually give way to mere force of habit. However, in doing so, the risks of remaining stagnant and losing motivation to commit to your duties can easily follow.
Stanford psychologist Carol Dweck, Ph.D., has written much on the topic of mindset. In several studies, she demonstrated how certain mindsets dramatically impacted performance. Particularly, a growth mindset — in which the person continually seeks to improve — was integral to participants’ long-term success. Similarly, a growth mindset can have tremendous effects on how a physician carries through with their work and views their job. In What Doctors Feel, a book by New York University physician Danielle Ofri, M.D., Ph.D., she discusses how a growth mindset in physicians not only improves patient outcomes but provides the additional benefit of mitigating physician burnout.
Lesson 3: Setting the tone is essential.
In my classroom, we would always spend at least a week at the start of the school year establishing the tone, or culture, of the class. On day one, rather than jumping straight into cells and molecules, we would discuss what the ideal learning environment could look like and brainstorm how we could achieve that together. The goal was to establish an inclusive, engaging and self-motivated learning culture that would permeate everything we did. In doing so, routine tasks that might have otherwise elicited groans became further opportunities for growth.
Similarly, in the hospital, I have seen how the culture of a team informs its practice. When an attending physician rotates onto a service and goes out of the way to establish a safe space, residents are usually able to adjust more quickly and, as a result, work more efficiently. When the senior residents and attending physicians are aware of the impact of developing such a culture, the result is usually a more cohesive and motivated work environment where everyone can invest in the same goals.
Note: John Choi is currently working on a book that would compile stories that highlight the similarities between teaching high school and practicing medicine. If this topic interests you or you have stories you would like to share, please either comment below or email him directly.
