There’s an old adage in boxing: “The punch that knocks you out is the one you don’t see coming.” While I lack the lived experience (thankfully) to confirm the veracity of this saying, it’s always made intuitive sense to me. Threats are most dangerous when we don’t expect them because we haven’t prepared to respond effectively.
In light of the deadly COVID-19 pandemic and the rise of antibiotic-resistant bacteria, it’s understandable that public health authorities are focused on addressing dangerous viral and bacterial pathogens. However, Fisher et al.’s compelling review article on the emerging threat of antifungal resistance in Nature Reviews Microbiology reveals that it may be prudent to consider another class of infectious threat — fungi.
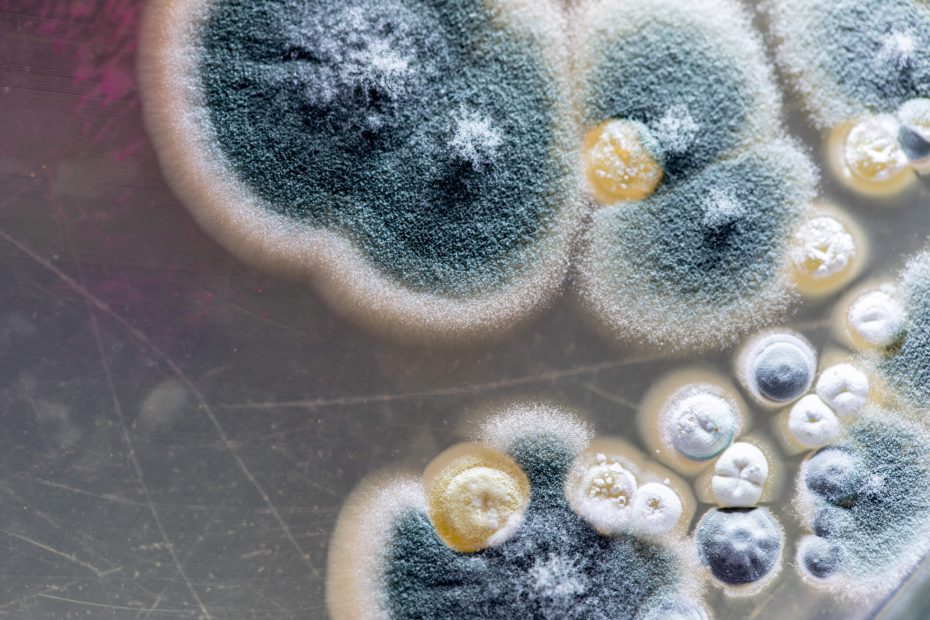
Fungi comprise an entire kingdom of life, including everything from the mushrooms in your backyard to the mold growing on the raspberries in your fridge. They are everywhere in the environment, and produce spores that we are all exposed to. While fungal infections may not be as prevalent or well-known as bacterial or viral infections, they already have had a significant impact on American health and health-care systems. A study of American hospitalizations in 2018 found that over 666,000 inpatient visits involved fungal infections, with an estimated total health-care cost of $6.7 billion. It’s also important to remember that this is likely an undercount of the true burden of fungal disease, as the CDC notes that fungal diseases are highly underdiagnosed.
Not all fungi can infect humans and cause disease, but many species can, and the severity of a fungal infection is often linked to whether an individual is immunocompromised. For example, cancer patients undergoing chemotherapy can acquire a serious Aspergillosisinfection. The Aspergillus fungus that causes Aspergillosis is frequently inhaled, is widespread indoors and outdoors, and, in vulnerable patients, can cause an invasive infection that spreads from the lungs to other parts of the body. Even in immunocompetent individuals, fungal infections such as Coccidioidomycosis, highly prevalent in the Southwestern U.S., can cause fatigue, cough and fever for weeks or months.
Unfortunately, our arsenal of treatments to address these often serious fungal infections is lacking. A major issue preventing effective therapeutic development is that fungi are eukaryotic, like humans, making it difficult to specifically target fungal cells. There are currently only four classes of antifungal drugs used in common medical practice, and sadly treatment failure and harmful drug-drug interactions are commonplace.
Our vulnerability to fungal infections is exacerbated by the rise of antifungal resistance. As fungi are exposed to antifungal drugs, fungi susceptible to said drugs are killed. However, over time, random mutations in fungal genomes inevitably provide mechanisms to evade treatment, whether through varying permeability of fungal cell membranes, inhibition of key enzymes or changes in binding sites. When these mutated fungi are exposed to antifungal drugs, their adaptations allow for survival, causing antifungal treatment failure. Thankfully, many fungal diseases cannot spread person-to-person, meaning that although the risk of transmitting these drug-resistant fungi cannot be excluded, the chances are relatively slim.
Unfortunately, the broad use of fungicides ecosystem-wide is leading to much more global antifungal resistance. Azoles are one of the four major classes of antifungals utilized to treat fungal infections, and studies have isolated azole-resistant Aspergillus fumigatus from the environment and from patients with no prior history of azole treatment. This means that people are being infected with fungi that are already resistant to antifungal agents, as opposed to naïve strains that acquire resistance upon treatment. This phenomenon is most likely due to the widespread use of agricultural fungicides.
Agricultural fungicides possess structural similarities to the antifungal drugs prescribed to patients, and are deployed in large quantities in farms around the world. Azole fungicide use quadrupled in the U.S. from 2006 to 2016 to a total of 3,000 metric tons annually. China is reported to use 30,000 metric tons annually. Further, the increased use of these azole fungicides corresponds to increased prevalence of azole-resistant human fungal pathogens, supporting the hypothesis that these fungicides are the culprit.
Fisher et al.’s review emphasizes that the ramifications of increasingly widespread antifungal resistance are concerning, as the process of adapting to antifungal molecules can also lead fungi to develop altered physiology that renders them more virulent or resistant to other drugs. Fisher et al. also note that climate change is an independent force driving fungal adaptations. Heat stress promotes fungal adaptation to warmer temperatures, which can alter antifungal resistance indirectly. Additionally, fungal adaptation to increased heat in the environment can allow for better survival at human body temperature. Critically, the growing threat of antifungal resistance is not theoretical. The CDC has issued a recent advisory regarding an increase in echinocandin-resistant C. auris, whereas Trichophyton indotineae possessing resistance to terbinafine antifungals has arisen as a public health threat in India.
This situation, while concerning, has promising solutions. Fisher et al. outline a number of key steps that can help, namely making significant investments in global monitoring for antifungal resistance, increasing research and development of new antifungal drug candidates, and improving stewardship of the use of antifungal drugs and fungicides. However, at a fundamental level, what’s necessary is a wake-up call. Fungal infections and antifungal resistance lack theattention and funding afforded to other infectious diseases that cause similar mortality, and that should change. It’s clear that fungi pose a threat, and that threat is only growing in magnitude.
In boxing, a punch may very well be most dangerous when you don’t see it coming. But in the case of antifungal resistance, punches are equally dangerous if we see them coming and do nothing about them.
Related Content
- ‘Tis The Season For Safe, Effective Vaccines
- A Viral Solution to Antibiotics Weakness
- The Cost of Preventing Pediatric Influenza Deaths
Want to read more from the Johns Hopkins School of Medicine? Subscribe to the Biomedical Odyssey blog and receive new posts directly in your inbox.