As a fourth-year medical student at Johns Hopkins, I have had the privilege of working with attending physicians in a number of outpatient clinics. My roles in the clinic have varied. In most clinics, I see the patient independently, take a history, and perform a physical exam. I then describe the course of the illness, medical history and physical exam to the attending physician, as well as share my assessment and plan for the patient. The attending and I then go and see the patient together. Other times, I am less involved in the clinic, perhaps only taking the history independently or shadowing. There are opportunities to write patient notes, ask questions and receive feedback, but the amount and quality of teaching vary between clinics.
In 2015, a group of Johns Hopkins medical students began investigating the factors that contribute to a successful outpatient educational experience for students in the neurology clerkship. They presented their findings at the American Academy of Neurology meeting last year. In collaboration with the neurology clerkship directors, they surveyed 67 students who took the neurology clerkship between 2014 and 2015. They found that students were significantly more likely to perceive a clinic session as an “effective educational experience” for each additional patient they interviewed, presented, and documented. In other words, students felt that they learn more when they are actively involved and have greater responsibilities.
In addition, the group also explored how students impact the clinical productivity of the attending physicians. This information is critical because of the widespread perception that medical students hinder clinical productivity, as attendings must juggle supervisory and teaching roles with patient care. Therefore, the group catalogued relative value units (RVUs), a metric for assigning value to clinical activities and a measure of clinical productivity, per clinic session with and without a student for 43 attending physicians.
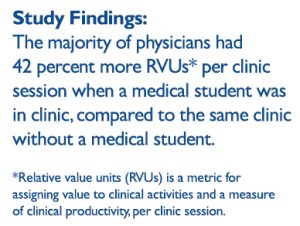 Surprisingly, the majority of physicians (74 percent; n=32) had 42 percent more RVUs per clinic session when a medical student was in clinic, compared to the same clinic without a medical student. This increase is most likely because in the time that the student sees the patient, attending physicians can simultaneously see a second patient or finish patient notes. Furthermore, the RVUs per clinic session significantly increased as the number of patients that students interviewed, presented and documented increased.
Surprisingly, the majority of physicians (74 percent; n=32) had 42 percent more RVUs per clinic session when a medical student was in clinic, compared to the same clinic without a medical student. This increase is most likely because in the time that the student sees the patient, attending physicians can simultaneously see a second patient or finish patient notes. Furthermore, the RVUs per clinic session significantly increased as the number of patients that students interviewed, presented and documented increased.
This study suggests that medical students can be actively incorporated in outpatient clinics in a way that is mutually beneficial for both the student and the attending physician. Students feel that they receive a greater educational experience when they are actively involved, and they can also increase the productivity of the preceptor.
One limitation in this study is that only neurology clinics at Johns Hopkins Hospital were surveyed. This work is still under review, but the next phase is to examine the generalizability of the conclusions across medical specialties and institutions. Currently, I am working together with Stephanie Zuo, another Biomedical Odyssey blogger, to extend this study to the pediatrics and women’s health clerkships at Johns Hopkins. Our hope is that this project can improve the outpatient educational experience for future medical students, as well as encourage attending physicians to participate in medical education.

Very interesting findings and great work. Get students in the clinic!
Comments are closed.