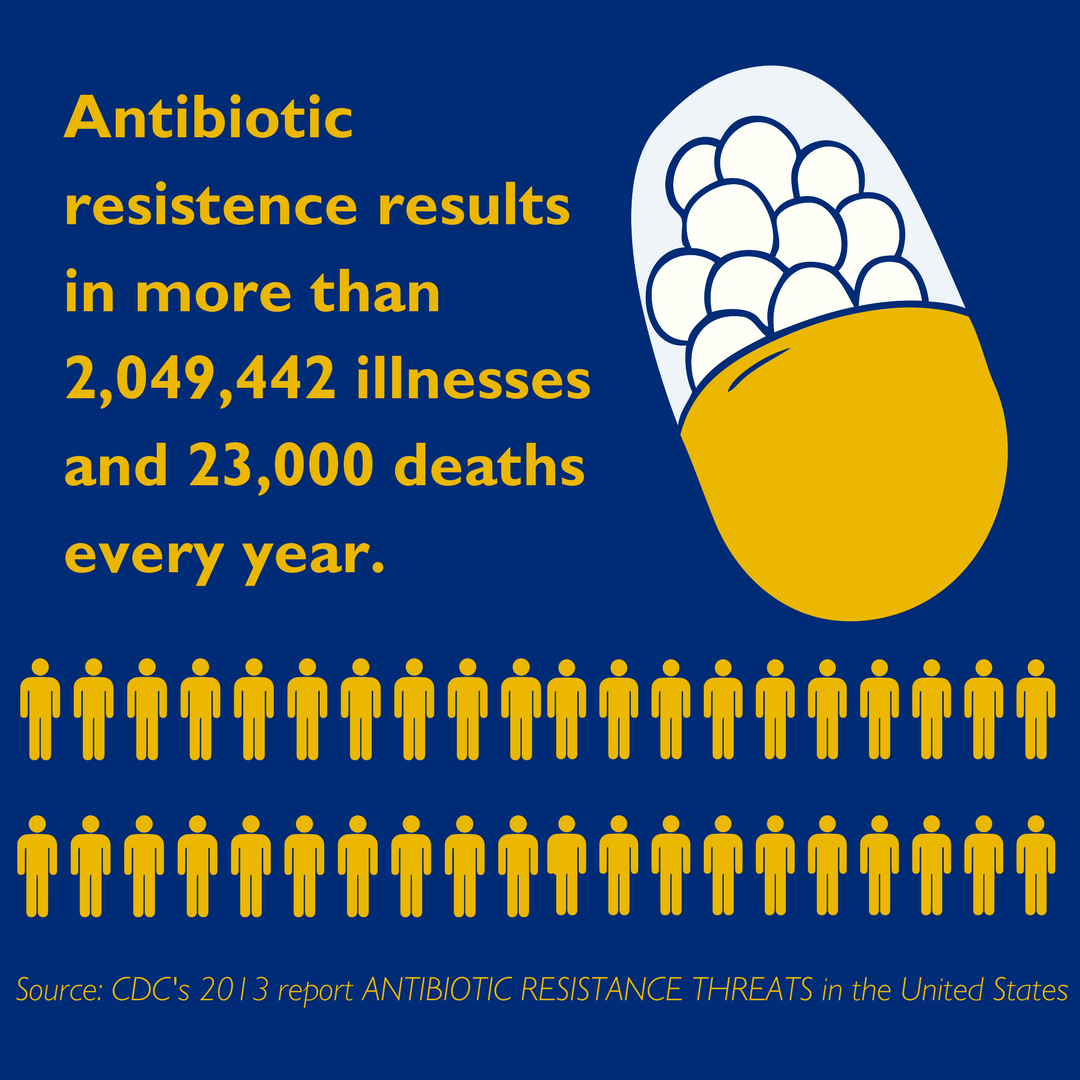
“...23,000 deaths a year.” “...over 2 million infections.” These headlines would be alarming but expected if they were descriptions of the latest Ebola outbreak. But alas, these are “conservative, minimum estimates” of antibiotic-resistant infections each year in the United States, as projected by the Centers for Disease Control and Prevention.
The Dangers of Antibiotic Resistance
Antibiotics are the lynchpin of modern medicine. Without their targeted efficacy against bacteria, minor surgeries are life-threatening endeavors; diseases we largely consider conquered, such as pneumonia and tuberculosis, become fatal again; and childbirth is a massive risk to mother and child alike. For many years, our arsenal of different classes of antibiotics has drastically improved the life- and health spans of humans across the world, by giving physicians an on-demand way to swiftly inhibit the growth of some of the most ubiquitous, and disease-causing microorganisms.
However, all life under selective pressure evolves and, over generations, bacterial strains have built a repertoire to evade, escape and denature these compounds. Of course, because of our society’s heavy reliance on antibiotics, the genes that confer resistance spread rapidly within the bacterial world and ultimately emerge as a new antibiotic-resistant pathogen. The most common examples are now household names, such as MRSA, or methicillin-resistant Staphylococcus aureus, the notorious scourge of hospitals and athletic facilities alike, or the recently emerged superbug CRE (carbapenem-resistant Enterobacteriaceae), among others. The root causes for this spread are multifold: overprescription of antibiotics, premature termination of antibiotic treatment by patients, and incomplete infection-control standards in high-risk areas like hospitals.
Optimizing the Use of Antibiotics
The problem of antibiotic resistance is clear to all in the medical field. The need for new classes of drugs is immense and pressing, but resistant strains are emerging rapidly, while development of new antibiotics has slowed dramatically. One strategy being utilized at Johns Hopkins to address these issues is the Antimicrobial Stewardship Program (ASP), a consortium of physicians and researchers tasked with developing guidelines to optimize the use of antibiotics in a hospital setting and ensuring patients receive the drugs they require, as a means to prevent the development and spread of resistant strains.
The ASP has been publishing comprehensive guidelines for antibiotic administration since 2001. As a team, the group synthesizes information from myriad doctors and researchers, both local and nationwide, to offer standardized suggestions for each antimicrobial agent as well as each use case. These guides are available to all physicians, who should then be able to optimize the drugs prescribed to each patient, while simultaneously combating the spread of antibiotic resistance writ large.
According to the ASP at Johns Hopkins, 30 percent of all antibiotics utilized in a hospital setting are incorrect or unnecessary. The litany of misuse includes overprescription and suboptimal antibiotic choice for individual cases. It is these types of situations the ASP hopes to rectify, and their guidelines are constantly being refreshed and revised using new information acquired from doctors’ experiences, as well as ongoing research on various outcome measures and improving delivery systems.
Unfortunately, even if the ASP is entirely successful and able to optimize antibiotic deployment to 100 percent efficiency, the rise of resistant strains will likely continue to seriously affect health care in both the immediate and long term. Until a new technology allows us to directly counteract infections, humans will always require drugs capable of specifically beating back the growth of disease-causing microbes. Although discovery of new classes of antibiotics has slowed considerably, a number of researchers have begun to search widely for new substances with antimicrobial properties. Like their predecessor, Alexander Fleming, these researchers are sampling diverse bacteria, fungi and other types of microbes throughout the world looking for endogenous, already-evolved bacterial defense mechanisms that can be tweaked or altered to build the next class of potent antibiotics for human use.
This will be an eternal battle. New antibiotics will be developed and used to further human health, while the organisms they are designed to kill will develop ways to evade them, and the predator-prey relationship continues. It is vital that the progress of new antibiotic research outpaces the emergence of resistant ‘superbugs,’ and this perpetual evolutionary race is why the ASP is so important now as well as far into the future.
Related Content
- Infections, Antibiotic Use Linked to Manic Episodes in People with Serious Mental Illness
- AHRQ Safety Program for Improving Antibiotic Use: Preventing patient harms today. Preserving antibiotics for tomorrow.
Pingback: Smarter Antimalarial Use: Altering Drug Duration to Improve Efficacy
Comments are closed.