While the word cancer treatment may identify everything from chemotherapy to radiation, there is significant variance between the type of cancer and its responsiveness to even the most promising therapies. That has been precisely the case for the α-PD-1 immunotherapy treatment. While it has shown remarkable efficacy in patients diagnosed with lung cancer, other types (such as ovarian cancer) do not respond as well.1 Cancer researchers are constantly trying to identify and refine treatment options and effectively target each cancer subtype. A group at the Johns Hopkins Sidney Kimmel Comprehensive Cancer Center has recently identified two FDA-approved drugs that work in combination with α-PD-1 to improve survival outcomes in a mouse model of ovarian cancer, showing a novel potential therapy regimen that could be further investigated in clinical trials.2
Immunity and Cancer
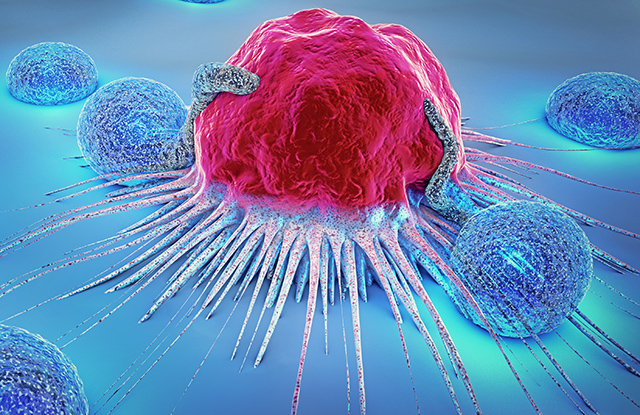
Cancer development centers on uncontrolled cell growth, which can affect how immune cells react to the growing tumor. In healthy tissues, signatures of abnormal growth are often present on the surface of cancerous cells, indicating their altered biology. These signatures are recognized and interpreted as warning signs by the immune system, which tries to respond by killing the cancerous cells before they are able to spread. In some types of cancer, such as epithelial ovarian cancer (EOC), the cancer cells grow in an immune-suppressed environment — in which the tumor evades the immune response by altering important immune cell interactions and impeding cancer cell death.3 These complicating factors make treating these cancers more difficult, as many therapies rely on the immune system to intervene.
Certain drugs, such as DNA methyltransferase inhibitors (DNMTis) and histone deacetylase inhibitors (HDACis), activate genes that help immune cells fight cancer cells, by increasing the number of immune cells recruited to the tumor environment and sensitizing cancerous cells to killing. These types of drugs are classified as epigenetic therapies because they alter gene expression without changing the underlying DNA sequence. The efficacy of epigenetic therapies in the context of ovarian cancer has not been extensively characterized and has not been investigated in combination with other cancer therapy drugs. The Zahnow group at Johns Hopkins recently published their findings on how exactly these drugs make ovarian cancer treatment more effective, and what the best combination is to improve survival in mice through epigenetic therapy.
Understanding the Immune System and Ovarian Cancer
The researchers wanted to identify the mechanism by which these classes of drugs act to reduce tumor burden and what each drug contributes individually to the therapeutic outcome. Using a mouse model of EOC, the researchers first treated cancer cells with drugs outside the mice, then injected the mice with the drug-treated cells and monitored cancer progression. They found that with a combination of HDACis and DNMTis there were more immune cells recruited and that in these immune cells, the anti-tumor signal was more strongly activated. This confirms what has previously been found in other cancer studies with these types of therapies.
Next, they treated the mice after they had been injected with untreated cancer cells, but in combination with the well-established immunotherapeutic treatment α-PD-1. Normally, α-PD-1 is not effective against EOC because the immunosuppressive environment of EOC seems to impede its activity on the limited immune cells present in the tumor environment. But in combination with the HDACis and DNMTis, the therapy not only decreased tumor burden but also increased the longevity of the mice by 14.5 days, on average.
To determine why exactly this therapy was so effective, the group blocked a receptor of a key immune signaling cascade — the type I IFN pathway — which is responsible for activating immune cells and recruiting them to the site of disease. When this pathway was blocked, the drugs were no longer as effective, with less immune cell activation and fewer immune cells recruited to the tumor environment. To specifically look at the contribution of the immune cells themselves, they tested the therapies in genetically modified mice that lack immune cells.
In this case, the DNMTi alone did appear to kill some cancer cells, even without those immune cells present. But the HDACi alone required the immune cells to be effective against the tumor. In other words, these drugs appear to rely on the actions of the type I IFN pathway mediated via immune cells to be most effective. This demonstrates the contributions of each drug and the pathway through which they work, as well as the individual mechanisms of action in ovarian cancer therapy.
Although the study was performed in mice, this type of combination therapy holds incredible promise for treating cancers such as EOC in humans. The HDACis and DNMTis helped activate signaling to the immune system and recruited more immune cells to the tumor microenvironment to better fight the cancer cells. This further improved a popular cancer therapy, α-PD-1, which offers an exciting way to repurpose drugs not always seen to be effective in cancers such as EOC. Such work is exciting and essential in the fight against cancer, giving researchers and patients new hope for more effective therapies.
References:
- J. R. Brahmer et al., Safety and Activity of Anti–PD-L1 Antibody in Patients with Advanced Cancer. New England Journal of Medicine 366, 2455-2465 (2012).
- M. L. Stone et al., Epigenetic therapy activates type I interferon signaling in murine ovarian cancer to reduce immunosuppression and tumor burden. Proceedings of the National Academy of Sciences, 201712514 (2017).
- C. C. Preston, E. L. Goode, L. C. Hartmann, K. R. Kalli, K. L. Knutson, Immunity and immune suppression in human ovarian cancer. (2011).