Finding new treatments for infectious diseases is often the focus of clinical research, but recent research has demonstrated the importance of both developing and improving diagnostic tools in the fight against malaria. Malaria is a disease caused by the parasite Plasmodium falciparum, and mosquitoes spread it. In 2017, there were over 219 million cases of malaria and over 400,000 deaths. Unfortunately, many of these deaths involved children under 5, whose still-developing immune systems are less equipped to fight the infection. With the right treatment regimen and use of preventive medication, malaria is both curable and preventable; however, it continues to persist throughout the world. Clinical symptoms are usually associated with the parasitic infection of red blood cells. Even mild infections can allow the parasite to replicate to a level where it can be taken up by mosquitoes upon feeding and thereby continue the cycle of transmission. Efforts to provide people with the best medicines, implement bed net usage and employ insecticides to cull mosquito populations have all contributed to a reduction in malaria prevalence in sub-Saharan Africa. But low-level infections can persist, even in areas with low malaria prevalence. These infections are particularly difficult to diagnose, even with very sensitive detection methods like PCR.
In diagnostics, sensitivity and specificity are key terms that researchers often discuss. Sensitivity refers to the ability of the diagnostic to correctly identify positive cases, while specificity refers to the ability to omit false positives. In other words, high sensitivity means a diagnostic will detect most of the true positive cases, and high specificity means the test will not accidentally diagnose someone who is not actually infected.
Properly diagnosing individuals is a critical first step in proper treatment, and current malaria diagnostics are limited. The rapid diagnostic test, or RDT, is very similar to a pregnancy test. A drop of blood is sucked into a membrane, which detects the presence of antibodies to malaria proteins. A small line will appear if there is evidence of an immune response against a malaria-specific protein, which for P. falciparum is called HRPII. If antibodies are present, this indicates a malaria infection by this parasite species. The trouble is, research has shown that this protein can persist in the blood, even after the infection has cleared. This reduces the specificity, and can make it difficult to determine whether or not a patient should be treated.
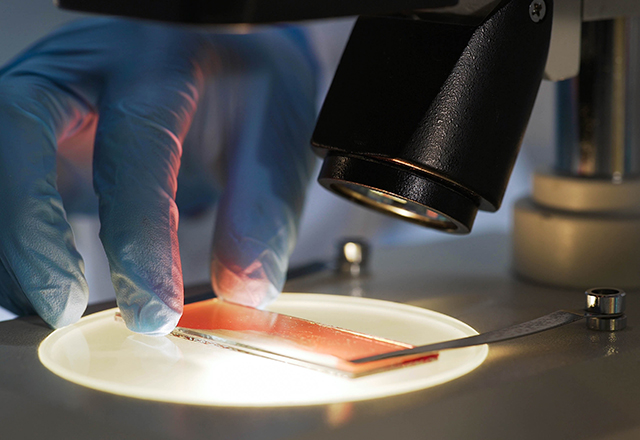
To better understand why HRPII persists after the parasite itself has been cleared, researchers at the Johns Hopkins Bloomberg School of Public Health used several models to better understand its behavior. Led by graduate student Kristin Poti, the study sought to examine the kinetics of how HRPII is cleared from the blood. To do this, they first looked at patient samples. Using blood from patients with malaria who were admitted to The Johns Hopkins Hospital, they separated the plasma and red blood cells from the whole blood, then used PCR to detect parasite DNA and used ELISA — a commonly used protein-detection technique — to measure HRPII. They could then compare parasite clearance, by DNA, and protein clearance, by ELISA. They also used fluorescence microscopy to examine individual red blood cells and look for HRPII in red blood cells with no current parasites. Through this method, they found that the protein actually remained in red blood cells after the parasites were cleared. They hypothesized that this phenomenon was possibly happening as a result of a process that takes place in the spleen, called pitting. Essentially, immune cells extract the parasite from the red blood cell, and the red blood cell remains intact and returns to circulation. But, the protein produced by the parasite is left behind in the red blood cell. This explains the persistence of the protein in red blood cells, but not the plasma, even after parasites are cleared.
Because patient samples are rare, the researchers then wanted to develop a mouse model to further study this. The parasite typically used in mouse models of malaria does not produce HRPII, so with the help of Amanda Balaban and the Sinnis Lab, the researchers created a parasite that infects mice and produces the P. falciparum HRPII. They could then look at HRPII production in mice during an actual infection and analyze their blood using methods similar to those used with the human samples. Again, they found that HRPII persisted longer in red blood cells than in the plasma, potentially due to HRPII persisting in pitted red blood cells.
To see if the spleen was having an impact on protein levels, they removed the spleens from the mice, then compared their HRPII levels to those in control mice that were also infected but did not have their spleens removed. The number of parasites and the levels of HRPII in asplenic mice were higher during the initial stages of infection. They found that in the mice without spleens, it took longer to clear parasite DNA, although HRPII clearance was very similar between the two groups over the first few days of infection. Low levels of the protein seemed to persist in mice without spleens. This could be because, without spleens, the parasites remain in red blood cells longer, thereby producing more HRPII. As the parasites are cleared by the immune system, and after drug treatment, that HRPII may remain in the cells. This highlights the importance of the spleen in infection clearance, and suggests that it may also play a role in protein clearance, but predominantly in the late stages of infection.
This study emphasizes the importance of understanding factors influencing diagnostics in order to make them more effective in the field. By examining the persistence of this parasite-specific protein, researchers were able to show that HRPII may be present even when parasites are not. This suggests that the diagnosis of malaria should rely not only on the RDT, but also use other methods such as PCR or microscopy to rule out potential false positives. Lingering levels of HRPII may complicate RDT specificity, especially in patients who have already been treated for malaria. Research such as this not only helps us to better understand the biology of malaria infection and how the immune system interacts with this parasite, but may also lead to improved diagnostics to further advance treatment of patients worldwide.