When I tell people I study platelets, I am not often met with excitement. Most people know platelets as those tiny things that form clots, and if they have a fully functional clotting cascade, they aren’t bothered that much about them. When I mention that I study how platelets play a role in the immune system, the reaction usually turns to confusion — clotting isn’t related to the immune response, is it? Well, not really. It turns out that platelets play several roles in the body, and during my postdoctoral fellowship at the Johns Hopkins University School of Medicine, I aim to learn more about how they work in the immune system in the specific context of HIV infection.
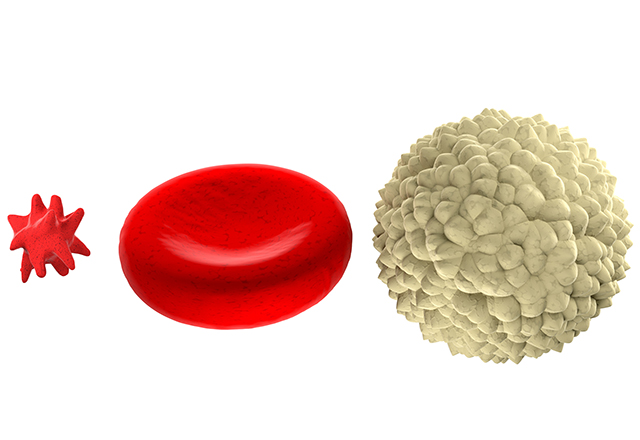
So, what even are platelets? To my understanding, they are very small cells. Many make the assertion that platelets aren’t truly cells because they lack a nucleus and are much smaller than most cells. However, (mammalian) red blood cells also lack a nucleus, and they have “cell” right in their name! Additionally, if red blood cells are any standard, a cell obviously does not need a nucleus to perform a vital job in the body. There is no dispute that platelets are very small. In humans, they’re around 2-3 microns in diameter — about a thousand times smaller than a grain of sand! Despite their small size, platelets are crucial for many physiological functions.
Platelets are formed from very large cells called megakaryocytes that are in the bone marrow. These large cells form long projections called “proplatelets” that pop off into the bloodstream and undergo some maturation steps before becoming full-fledged platelets. As platelets get older and more mature, they shed extra volume and become more compact. That’s why, if a CBC (complete blood count) is run on blood, it reports both the platelet number (usually abbreviated PLT) and the platelet volume (reported as MPV or mean platelet volume). Having a higher MPV indicates that a person or animal has larger circulating platelets, meaning their bone marrow is producing a lot of new, “young” platelets and pushing them right into the bloodstream. This often occurs if an individual has a bleeding event. Interestingly, the life span of a platelet in the human bloodstream is seven to 10 days, which means the bone marrow responds very rapidly to bleeding events to produce these new platelets.
Platelets are, famously, very important in the clotting cascade — what happens when an individual has a bleeding event. They detect a breakdown in the blood vessel’s structural integrity — like a hole. They grab onto that area with fingerlike projections that stick off their surface, and recruit more platelets to form a plug in the hole to prevent further leakage. A cool thing that many people don’t realize is that a system opposes the clotting formation system — a system designed to prevent clots from getting bigger and to break down clots that have formed. This system is very important for restoring normal blood flow after the blood vessel is healed. You wouldn’t want old blood clots hanging around forever in all your vessels that have ever been injured!
But platelets are not just vital for keeping blood inside the blood vessels. Platelets also play a role in the immune system, by working with the cells that line blood vessels and with other immune cells in the bloodstream. In certain disease states, including dengue fever and malaria infections, platelets can bind to the blood vessel directly and make it a weaker barrier. The vessel then allows more cells, including white blood cells, through the vessel and into the tissue to fight the infection. Blood vessels are in all of our tissues to supply oxygen and nutrients, so decreasing their barrier strength selectively is an important part of platelet function — if you have, for example, an infection in your kidney, you would want extra white blood cells to get into your kidney, but not necessarily your heart or lungs! This can have a positive or negative function — allowing white blood cells into a tissue where infection is lurking can mean the immune system has a better chance at fighting that infection, but decreasing the barrier strength may also allow infectious agents access to the tissue. Platelets can also interact directly with white blood cells in vessels, by grabbing onto them and helping them pass into tissues or by changing how they then interact with other cells or infectious agents they encounter in the future.
My project at The Johns Hopkins University focuses on what effect platelets have on blood vessels in the brain in people living with human immunodeficiency virus (HIV). HIV attacks and infects the white blood cells in the body and can lead to AIDS (acquired immune deficiency syndrome) if untreated. We know that these individuals are more likely to have neurocognitive dysfunction than people who are uninfected, with issues falling into a group collectively called HAND (HIV-associated neurocognitive disorders) that can impact fine motor skills or speech processing and may progress to dementia. Unfortunately, even with highly effective antiretroviral therapies that prevent HIV from replicating itself and harming the immune system, HAND has continued to affect a high proportion of people living with HIV, and no effective therapies have been developed yet. We want to know if platelets play a role in this dysfunction by decreasing the strength of the blood-brain barrier, one of the tightest and most secure blood vessel barriers in the body.
Platelets are really interesting little cells, containing many factors that they can release into the bloodstream to call other platelets and blood cells to areas of distress. I hope my work here can increase our knowledge about these tiny warriors fighting on the front lines of blood vessel damage and immune function!
Related content
- In Search of a Cure for Tissue Injury: The Rise of Mesenchymal Stem Cells in Regenerative Medicine
- Platelet-Rich Plasma: An Emerging Therapy for Musculoskeletal Injuries
- A New Blood Test Tries to Detect Cancer Sooner
Want to read more from the Johns Hopkins School of Medicine? Subscribe to the Biomedical Odyssey blog and receive new posts directly in your inbox.