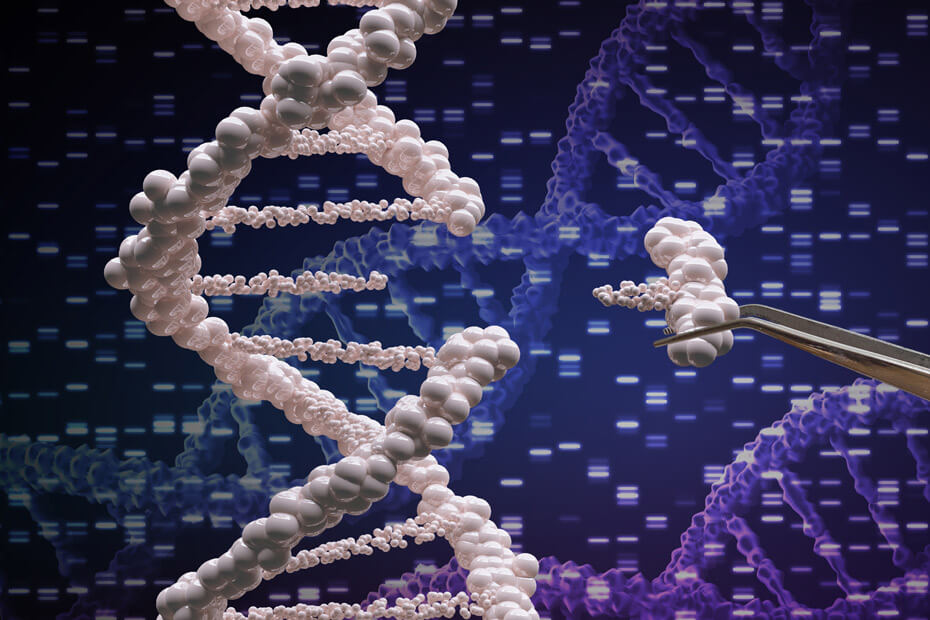
The power of genetic editing as a therapeutic strategy has long been appreciated, but the risk of unintended and unknown side effects has kept it out of the clinic. With the Food and Drug Administration’s recent approval of a CRISPR-based approach for treating sickle cell anemia, wider acceptance may spark a new era in medicine.
Clustered regularly interspaced short palindromic repeats sequences (CRISPR), along with many classes of CRISPR-associated (Cas) proteins, evolved as an ancient protective mechanism for prokaryotic organisms (i.e., bacteria and archaea) to fight off invading viruses. When foreign DNA is detected, Cas proteins cut out small portions of this genetic material and insert them into a CRISPR array in the prokaryotic genome. CRISPR sequences are transcribed into ribonucleic acid (RNA), which forms a complex with other Cas proteins. CRISPR/Cas complexes can then bind to and degrade matching viral DNA sequences to prevent subsequent infection
In 2012, researchers demonstrated that CRISPR could be programmed to target precise genetic sequences by designing guide RNAs (gRNAs) for specific sequences of DNA. This approach is often used to knock out a protein by eliminating its expression, but it can be modified to alter the genome and epigenome. For example, by pairing a gRNA with a corrective template sequence, the CRISPR/Cas system can be used to change the genetic code.
When CRISPR-based genetic editing was first described, the prospect of its use in research or in treating human disease raised many ethical concerns. However, in November of last year, the U.K.’s Medicines and Healthcare products Regulatory Agency authorized the first use of CRISPR gene-editing therapy. The drug, Casgevy, was also approved by the FDA a few weeks later.
Casgevy, developed by Vertex and CRISPR Therapeutics, treats sickle cell disease and β-thalassemia, both of which are caused by abnormal production of hemoglobin. Using stem cells extracted from patients’ bone marrow, Casgevy targets the BCL11A gene, allowing cells to generate fetal hemoglobin, which has a higher affinity for oxygen. Also, its unique sequence prevents it from polymerizing with disease-associated hemoglobin, thereby preventing red blood cell sickling and decreasing symptoms of sickle cell disease. In both U.K. and U.S. clinical trials, more than 90% of those who were treated for both sickle cell disease and β-thalassemia had a positive outcome, and there were no significant safety concerns.
Now that CRISPR has achieved the essential regulatory milestone of FDA approval, the possibilities for future drug development are vast. Perhaps the most tractable application would be using CRISPR for other “single-gene disorders,” such as cystic fibrosis or Huntington’s disease, which are thought to develop due to dysfunction of a single protein. If CRISPR can establish itself as being safe and effective in humans in these narrow cases, this ancient molecular machinery could find fresh use.
Related Content
- Genome Engineering Emerges from the Shadows
- How Genetics Can Inform Future Missions to Mars
- Johns Hopkins Tackles Genome Editing with CRISPR/Cas9 Symposium
Want to read more from the Johns Hopkins School of Medicine? Subscribe to the Biomedical Odyssey blog and receive new posts directly in your inbox.