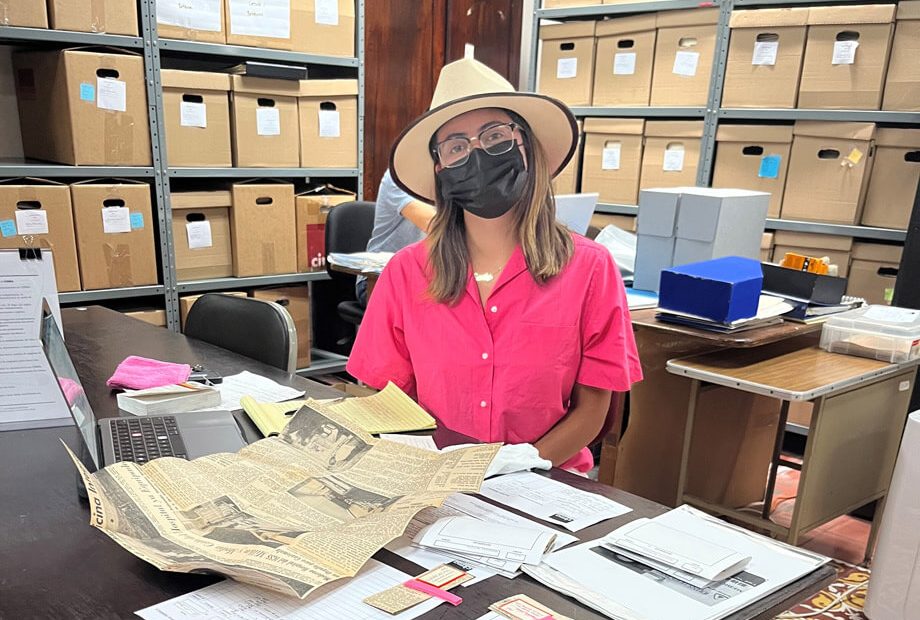
Make Time to Stop and Smell the Flowers: Cherry Blossoms in Baltimore and D.C.
Photos courtesy of the author. One of the most beautiful parts of spring here in the mid-Atlantic is the return of the cherry blossoms. In… Read More »Make Time to Stop and Smell the Flowers: Cherry Blossoms in Baltimore and D.C.