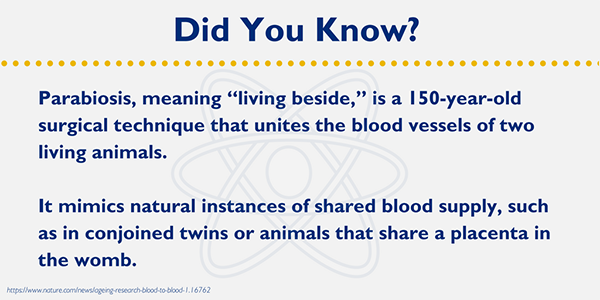
Anticipating the Unexpected: What is Your Plan for When Life Goes Awry?
“The best laid schemes of mice and men…” begins the oft-quoted line by Robert Burns, with usually no need to finish with “…go often awry.”… Read More »Anticipating the Unexpected: What is Your Plan for When Life Goes Awry?